Periodontitis Treatment
Periodontitis treatment and answers to frequently asked questions about the disease
The primary function of the teeth is to chew food. For this, they must be properly ‘fixed.’ A complex of tissues called ‘periodontium’ is responsible for the reliable fixation of the teeth. All elements of the periodontium, which include the gums, interdental ligaments, and the bone bed of the tooth, are interconnected. Changes in any part inevitably lead to changes in the rest of the components of this complex system. Periodontitis is an infectious inflammatory process in the periodontium tissues. Such a disease is quite widespread. According to statistics, most of the population suffers from it. Periodontitis usually affects middle-aged and elderly people, but recently the disease has become increasingly common in young people.
According to the global statics, periodontitis is a principal cause of tooth extraction!
Periodontitis symptoms
Periodontitis is called ‘a silent teeth killer.’ At the initial stages, the disease is asymptomatic, without acute painful sensations. As a result, patients often do not pay attention to the bleeding of the gums that occurs from time to time. However, it is in the initial stage the disease can be treated. Pronounced symptoms (teeth mobility) occur most often when the teeth cannot be saved. At later stages, periodontitis cannot be completely cured. You can only slow down the process of its further development.
Classification of periodontitis
Depending on the complexity, the disease is divided into several types:
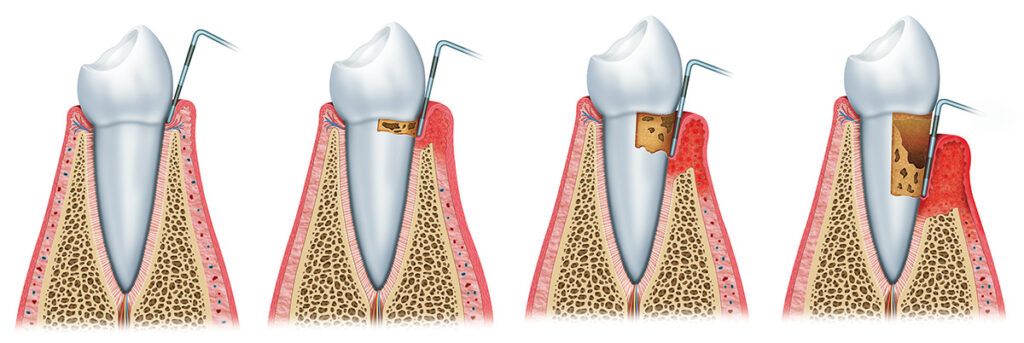
- Light degree. As a rule, the disease begins with gum inflammation, known as gingivitis. Typical symptoms are swelling and redness of the gums and their bleeding due to mechanical irritation, such as brushing teeth or eating solid foods. At this stage, tissue damage is reversible, since the process has not yet affected the interdental ligaments and the jawbone.
- Moderate degree. If measures are not taken on time, the infection spreads deep into the gums and destroys the ligaments that hold the teeth. The gum begins to flake off. Between the gum and the wall of the teeth, the so-called ‘pockets’ become deeper, making gaps that accumulate with bacteria. Their depth, which is normally 3 mm, increases to 6 mm. The gaps between the teeth widen, bad breath appears, and the gums become loose and begin to bleed constantly.
- Severe degree. Further progress of the disease leads to the lowering of the gums and exposure of the dental necks. The depth of the gingival pockets can be up to 7-10 mm. The teeth become extremely sensitive. In addition to blood, purulent discharge appears. The jawbone, to which the teeth are attached, begins to collapse. Teeth lose stability, loosen, and fall out. In some cases, with a severe degree of periodontitis, the temperature may rise, and overall health deteriorates.
Causes of periodontitis
The leading cause of the appearance of periodontitis is poor oral hygiene. Plaque not removed in time accumulates and turns into tartar, which irritates the gum mucosa and provokes inflammation. This factor in the onset of the disease is the most common, but it is not the only one. Besides that, the occurrence of periodontitis is caused by an uneven load on the teeth. It can occur because of an incorrect bite and unrepaired spaces in the dentition. Reduced blood supply to the gums, which often results from the predominance of soft foods in the diet and smoking, is another cause of the disease. Mechanical trauma to the gums. Inherited predisposition. Unbalanced diet, deficiency of vitamins of groups A, B, and C, lack of calcium. Allergic and infectious diseases, as well as chronic diseases of the gastrointestinal tract, cardiovascular and endocrine systems, can also result in periodontitis.
Diagnostics
- Clinical evaluation (Examination of the teeth and gums, combined with an examination of the pockets and measurement of their depth, is usually sufficient to make a diagnosis. Pockets deeper than 4 mm indicate periodontitis)
- Dental X-ray: orthopantomography, CAT scan (detection of alveolar bone loss)
Periodontitis treatment
For problems with teeth and gums, only comprehensive treatment of periodontitis can help. It will depend on the severity of the stage of the disease. It includes several steps:
- Prevention
- Periodontitis treatment.
Treatment of periodontitis depends on the degree of the disease and is based on the individual clinical case. The primary emphasis is placed on removing tartar from under the gums and on improving oral hygiene. The necessary antibiotics, vitamins, and antiseptics are prescribed. In case of severe periodontitis, surgical intervention is needed. It includes the curettage of pockets and osteoplastic operations to restore bone. Patients with periodontitis are advised to use brushes with stiff bristles, which remove plaque better. At first, the gums’ bleeding can increase, but over time, the gums will get used to the new cleaning regime. Accurate and timely diagnosis plays a significant role in the prevention of periodontitis. Get a preventive dental check-up every six months. The specialist can recognize the problem early, prescribe timely treatment, and prevent its development. Be sure to go through a professional teeth-cleaning procedure to remove plaque and tartar effectively. Of course, proper and regular oral care is the basis of prevention you may consider.
- Plaque removal, cleaning of tartar: ultrasonic, Vector-therapy, laser, mechanical method.
- Series of treatments – drug-induced applications, PRP therapy.
- Providing hygienic instructions to the patient
- Sanitation of the oral cavity: filling of carious cavities, removal of damaged teeth, wisdom teeth, elimination of defects in prosthetics. At this stage, it is necessary to eliminate sources of infection.
- For moderate and severe forms, surgical treatment is indicated.
- Correction of bite, splinting of teeth to eliminate mobility, and prevent loss.
Periodontitis and implantation
With periodontitis, a paradoxical situation often arises. The disease leads to the loss of teeth, but it also prevents their restoration. It is impossible to fix the prosthesis on mobile and weakened teeth. Classical implantation with periodontitis is often impossible since the disease is accompanied by a rapid decrease in the volume of bone tissue, which is necessary for reliable fixation of the implant. Today, modern technologies allow us to restore missing teeth even with bone atrophy and inflammatory processes of the gums. Modern implants of special design can also be installed in case of periodontitis. In a particular clinical situation, the ‘all in 4/6’ technology is actively used. The implants are placed in specific points of the jawbone that are least susceptible to changes. The prosthesis is installed on such reliable supports. In some cases, bone augmentation is also performed. The service life of modern implants is 10 years or even more. The clinical survival rate is at least 95%. You can get more detailed information on the topic by scheduling a consultation with the specialists of Denta Vita.
